Tech tools, action plans help de-escalate thoughts of suicide
Published on Sunday, July 1, 2018
By: Ruth Cummins
The American Foundation for Suicide Prevention’s 2018 data for Mississippi shows that on average, one person dies by suicide every 23 hours in the state.
Suicide is the 13th-leading cause of death in Mississippi and the third-leading cause for ages 15-34. And that doesn’t include suicides that go unreported.
Those statistics may be alarming, but experts at the University of Mississippi Medical Center say there are tools for coping with extreme distress that often leads to thoughts of suicide. Just as importantly, they say there are resources available to create an action plan for when intense feelings escalate.
“Extreme emotions don’t last forever,” said Dr. Courtney Bagge, an associate professor of psychiatry at UMMC whose specialties include suicide, its treatment and its prevention. “Because episodes of extreme distress are almost always brief, temporarily putting space between yourself and the means of self-harm can save a life.”
She said individuals experiencing emotions that have brought them to the brink of attempting suicide “need to call 911 or a crisis line, or have somebody else do it. Ditto for taking those steps for someone you know.”
“You might have thoughts of not wanting to be here anymore,” she said. “It might only happen occasionally, but having a plan for what to do when those thoughts occur can help you stop them from escalating.”
She said it’s important to note the majority of people who have suicidal thoughts don’t die by suicide. By getting help, “there is hope, and they can go on to live healthy, meaningful and productive lives.”
Bagge said there are specific actions individuals can take and resources they can lean on to help them cope with increased distress and de-escalate emotions that are running high.
“The goal is to help you move from a ‘hot moment,’ where maybe you can’t even think, to a ‘cool moment,’ where you know, even though things may feel hopeless, you can get through it,” she said. “Suicide crisis lines are available 24/7 and staffed by compassionate counselors trained to help those in extreme distress.”
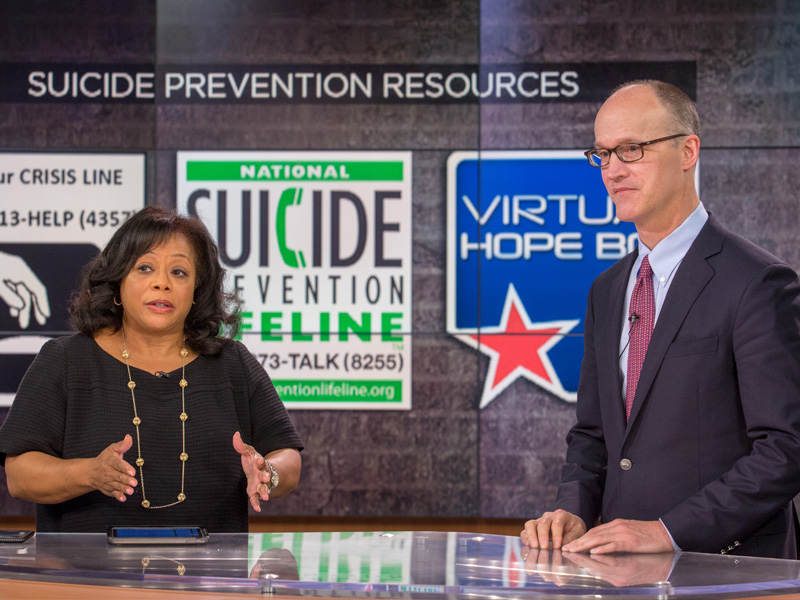
Individuals can confidentially call the toll-free National Suicide Prevention Lifeline at 1-800-273-TALK (8255) or locally, the Jackson Crisis Line at (601) 713-4357.
Crisis lines aren’t just for those who are actively contemplating suicide, however.
“They’re a wonderful resource for discussing not just suicide, but painful emotions,” Bagge said. “It’s something I talk to my patients about. People who are worried about someone can also call for information about how to help.”
She said those who need immediate help, advice or a listening ear also can use their smartphones to text or have a web chat with experienced suicide prevention counselors. Individuals can text “HOME” to 741741 and familiarize themselves with the chatroom before a crisis here. They can take part in a Lifeline live chat here.
“I encourage everyone and anyone to put these resources into their phone, and for the text, there’s a setup process,” Bagge said. “When you’re in a distressed state, for yourself or others, that’s not something you are able to do.”

Another key resource is the free Virtual Hope Box app, Bagge said. Users of the app can click “distract me,” “relax me,” “inspire me” and “coping tools,” and they can upload important photos, quotes or other images that can uplift them by clicking “remind me.”
Outside of crisis hotlines, not everyone is familiar with technology tools, though. Christina Jordan of Tupelo lost her 18-year-old son Gabriel when he took his life in 2014. Although she spent years getting Gabriel professional help, she said she wishes she’d had more resources to draw on as her son struggled with depression and suicidal thoughts.
“There are services available now that I didn’t know about with my son,” Jordan said. “I believe that could have made a difference.”
“It’s often difficult to find the help you need, depending on where you are and where you live. In Mississippi, it can be a challenge,” said Dr. Scott Rodgers, professor and chair of psychiatry and human behavior. “A psychiatrist like me would be helpful, but there aren’t many of us around Mississippi, especially child psychiatrists.”
Bagge offers four coping strategies to de-escalate distress during day-to-day anxiety and depression or before suicidal episodes.
• Take medications daily; eat and exercise regularly; and avoid alcohol and substance abuse.
“I tell my patients that a lot of times, you don’t want to eat, but make sure you eat something every four hours. By making sure that you are eating, being active and taking your medicines, it’s giving you the best chance to not react as strongly when you experience negative events.
“If you are depressed, alcohol or substance abuse makes it worse. I tell patients that until they are stabilized in treatment with a combination of medications and therapy, not to drink alcohol. It can make you focus more on the negative situation and not be able to focus on the buffers that would stop you from reacting, or stop you when you are considering suicide.”
• Create distractions, such as mindful breathing, going outside or focusing on the little things, and practice them before entering a distressed state.
“Breathe in deeply through your nose, fill your belly with air for three or four seconds, then exhale. You’re focusing your mind on the breathing and it can be incredibly helpful in centering yourself.
“It’s hot outside, but feeling the sun on your face is a good thing. Don’t eat at your desk. At least go sit by a window. Go to (a shopping area) and watch people. Walk around the block. It gets you out of your head. If you’re overwhelmed in your home, do one task that would take 15 minutes, like a load of laundry. You will feel accomplished, but it’s not a huge thing for you to do.”
• Change the temperature.
“Hold ice in your hand and notice it melting. It’s hard to think when you are holding ice. Put an ice pack around your nose and eyes, and hold it there. It will slow everything down. It sounds scary, but getting into a cold shower will shock your system and slow it down.
• Call a friend, not necessarily to tell them of the distress, but as a distraction.
“This can be someone from church or your synagogue, or a sponsor of some sort,” she said. “It could be a coworker or acquaintance.”
Her advice to friends and family: Don’t just tell a suicidal person he or she need help and leave it at that. And lock all guns and ammunition in separate locations.
“Listen non-judgmentally, take them seriously and remind them that you are there to help,” Bagge said. “Help them to get into treatment. Help them to make the appointment. It’s not easy to take these steps alone.
“Take them to the emergency room. People should be responsive when their loved ones talk about suicide or emotional difficulties, just like they would about diabetes, heart attack or stroke.”
Rodgers said depression and anxiety are chronic illnesses.
“They’re treatable,” he said. “Patients can be very well managed and lead happy, productive lives.”
Bagge said most suicides in this country involve a firearm, usually one that belongs to a family member. If someone is actively exhibiting warning signs of suicide, “our recommendation is to temporarily remove the firearm from the house,” she said. “We know this can reduce suicide. With a firearm, there’s usually not a chance to recover.”
She said to use both professional resources and coping mechanisms to get ahead of emotions that can escalate.
“It’s important to have a plan in place and places you can go to provide distractions, day or night,” she said. “Too often, we think of the end game. If we can notice when our negative emotions are increasing and we can use some coping strategies at that moment, it might not escalate to a crisis on that day.
“It’s about using strategies, farther up a chain of events or feelings, that can help you in the moment, and not waiting until when you are thinking about killing yourself.”



